Good hygiene includes never touching ones face or a patient with unscrubbed hands.
Flukes of nature do happen. Flukes in caregiver behaviour should never happen.
Nature has many flukes. It’s natural. So too is the entire Universe. Did you know that most scientific theories on creation assume the Universe is based on a measure of entropy (chaos or randomization).
Circles are never perfect; DNA has flaws; squares are seldom square; up is sometimes down. These are the pretty imperfections of the Universe.
Anomalies occur in humans and in fact within every sentient being.
Anomalies occur in microorganisms. One cannot always predict their behaviour. That’s bad when it comes to microorganisms humans must consider as enemies. That’s what we are going to talk about in this article.
Message to members, administrators and medical practitioners of RINJ Foundation and all partners.
By Micheal John
Notes: This article introduces some training resources. This is not a directive but new directives have been issued. Check your documents directory and group folders for new medical directives regarding the current COVID-19 outbreak. There will be more as new information becomes available and new requirements are indicated. We share this information for members who are not practitioners but realize it may not all apply. Questions will be quickly answered via email or Whatsapp to +16477399279
Who will get the COVID-19 illness? Some people call this “luck”, both good and bad. There’s no such thing. Randomization has patterns and it has keys.
- What I want you to do for yourselves is mitigate or abandon that concept.
- Don’t rely on luck. Be prepared for every eventuality within your scope of practice and know what you will do and where to consult for events outside your scope.
- Always know who will be your “go-to” person for escalation of cases or requests for information for which you have no procedure.
- Know what to do in your environment in the event of a sterilization breach.
- Always have a knowledge-based predetermined alternate plan of action for everything you do. In most cases this will be to consult a peer or to escalate to a supervisory peer.
- Never break a safety rule for expediency sake.
- Put your own safety first as an example to all others because as a leader, with people following you, your steps must be toward safety and good health.
COVID-19 is an enemy that must be first suppressed and then, maybe by scientists, maybe by you, defeated.
While you work toward suppressing this virus, the best way ahead is to deny it any hosts. That includes denying it access to yourself.
Your safety is your first job of work. Take no shortcuts that risk the safety of caregivers. That’s not how to save lives or to provide care to the ill.
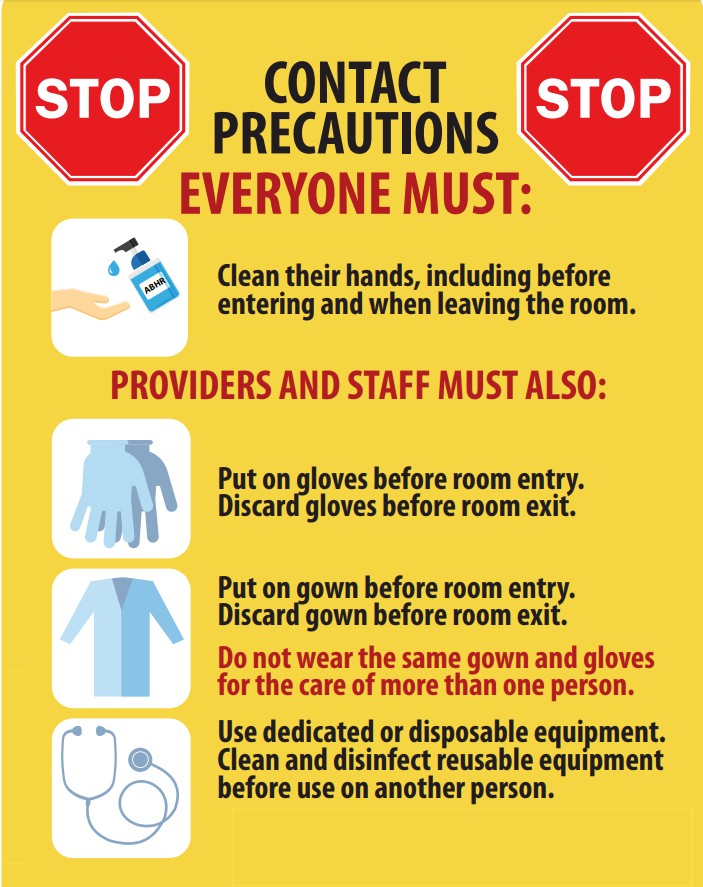
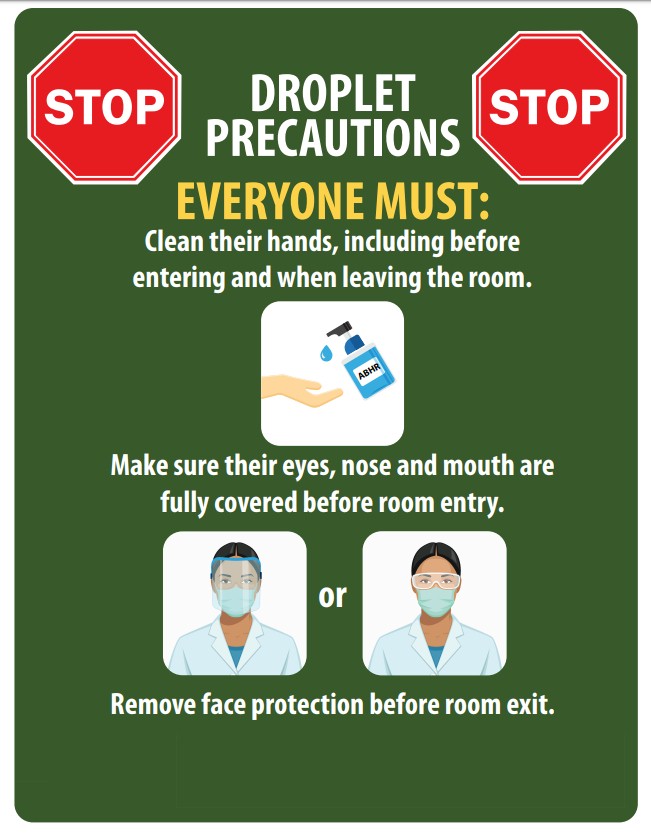
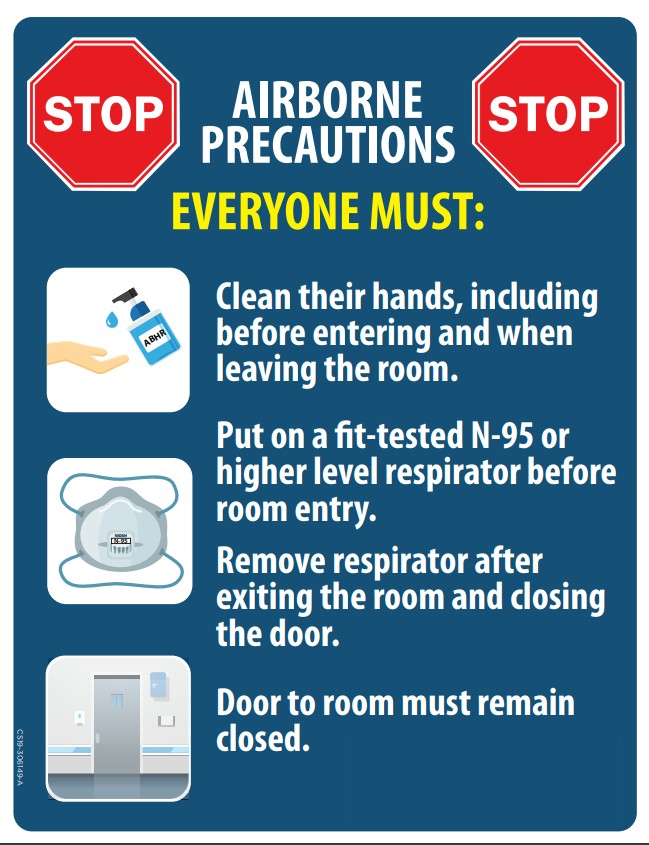
In suppressing this pathogen by denying it hosts, be concerned most about its ability to survive by adapting. That means adherence to the rules of sterilization, infection control for contact and airborne pathogens.
Remember that the COVID-19 pathogen wants access to respiratory systems and that it can probably get there through any orifice of a body. Good hygiene is important for patients and for caregivers. Good hygiene includes never touching ones face with unscrubbed hands.
This must be stressed for outpatients. Be aware of local regulations and apply local government rules.
The pathogen’s goal is basically, make an infinite number of self copies. It will use human bodies to do that as well as any animal species it can invade to become its host.
Disallow the enemy all hosts.
COVID-19 can live in feces, spit, nasal drainage and lung debris. Patients need to be trained to cough or sneeze into the crook of their arm or disposable paper tissue. They must also know the rules for disposal and hands scrubbing after each event.
Handwashing with a good soap for a minimum of 20 seconds must be accomplished regularly and both before and after any bare hand contact with any surface. Practice good sterilization while using personal protective equipment.
Patients can become infected again. Please dispel any beliefs that the human body can develop antibodies that prevent reinfection. The rigid rules for hand washing may become a a norm for human existence. Hand sanitizers are acceptable alternatives until proper handwashing is available.
Remember also that alcohol based cleaners are not very thorough and will not kill all coronaviruses. Here is a brief from one of our suppliers. There are many brands but actually just a limited number of truly effective chemical combinations. Fallow your facilities’ guidelines but use good rule-based logic and common sense for your own safety. Handwashing with a good soap is hard to beat. Facilities cleaning is usually decided by facility administrators.
| Quaternary Ammonium Compounds (Quats) | A top choice for disinfection in hospital and institutional settings because of their low cost and quick action against a wide range of microorganisms. Quats can be formulated with a variety of detergents to provide both cleaning and disinfecting ability. Nyco’s Ever-Pine disinfectant is an example of a quat-based disinfectant with both cleaning power and broad spectrum kill claims for many common and dangerous bacteria and viruses. |
| Chlorine Compounds | Kill an array of organisms including resistant viruses, and are highly recommended for cleaning bodily fluids. Chlorine-based disinfectants are inexpensive and have relatively quick kill times, however they can be corrosive and cause discoloration as well as irritation if not used as directed. Chlorine Sanitizer II is an example of a chlorine disinfectant, ideal for use in healthcare settings and food preparation processing. |
| Alcohols | When diluted in water, alcohols are effective against a wide range of bacteria, though higher concentrations are often needed to disinfect wet surfaces. The downsides are they evaporate quickly (and thus may not remain on the surface long enough to kill), they’re flammable, and they may not have organic soil tolerance claims, meaning they may not be effective when organic matter (blood, for example) is present. |
| Aldehydes | Very effective against the bacteria that cause Tuberculosis, yet they need a high part per million (ppm) ratio to be effective for disinfection. Some bacteria have developed a resistance to aldehydes, and have been found to cause asthma and other health problems. They can also leave greasy residue and must be in an alkaline solution. |
| Iodophors | Can be used for disinfecting some semi-critical medical equipment but they can stain surfaces and have an unpleasant odor (think Iodine). Idophors aren’t often used in facility maintenance anymore. |
| Phenolic Compounds | Effective against pathogenic bacteria including Mycobacterium tuberculosis as well as fungi and viruses, but also very toxic and corrosive, attacking surfaces while they attack the organisms on them. Some areas enforce disposal restrictions on Phenols. |
| Hydrogen Peroxide | Often mixed with peracetic acid to achieve specific disinfecting claims. These strong oxidizers can be highly reactive if mixed with other chemicals or come in contact with various surfaces. Their efficacy range is somewhat limited and at high concentrations they are dangerous. All in all, there are much better choices than hydrogen peroxide for facility disinfecting. |
As the human body builds its defences, the pathogen grows a shell; or changes its preference of receptor or chooses other human cells; or it reaches into its DNA and pulls out another trick. It is predictable that the COVID-19 pathogen will continue to evolve in order to survive.
Frankly, the COVID-19 is particularly nasty, like the influenza strains, it can make people very sick and cause their quick but traumatic death. Septic shock is one of the final stages. This thing is cruel. The victims are randomized but the majority are males from middle age to the elderly.
The COVID-19 disease is a very close cousin of the SARS pathogen. It’s in the same family as MERS. It is also spotted in the animal kingdom very often in recent years, not exactly, because it adapts to its environment to survive.
Information for Nurses and other health professionals
Healthcare personnel should adhere to Standard, Contact, and Airborne rules and precautions, including the use of eye protection (e.g., goggles or a face shield) when caring for patients with COVID-19 infection. These precautions include the use of PPE, including NIOSH-approved N95 respirators, gowns, gloves, face shield/eye protection, etc. This includes, but is not limited to, surgical N95 respirators.


Healthcare personnel can protect themselves when caring for patients by adhering to infection prevention and control practices, which includes the appropriate use of engineering controls, administrative controls, and personal protective equipment (PPE). The USA CDC has issued guidance recommending the use of PPE for healthcare personnel caring for patients with confirmed or possible SARS-CoV-2 infection. Employers and healthcare personnel are reminded that PPE is only one aspect of safe care of patients with COVID-19.
Nurse Work Area / Locker Signs
Some reminders from our sisters in Singapore on the care and use of N95 Respirator Masks which you will be wearing for most minutes of your lives for the foreseeable future
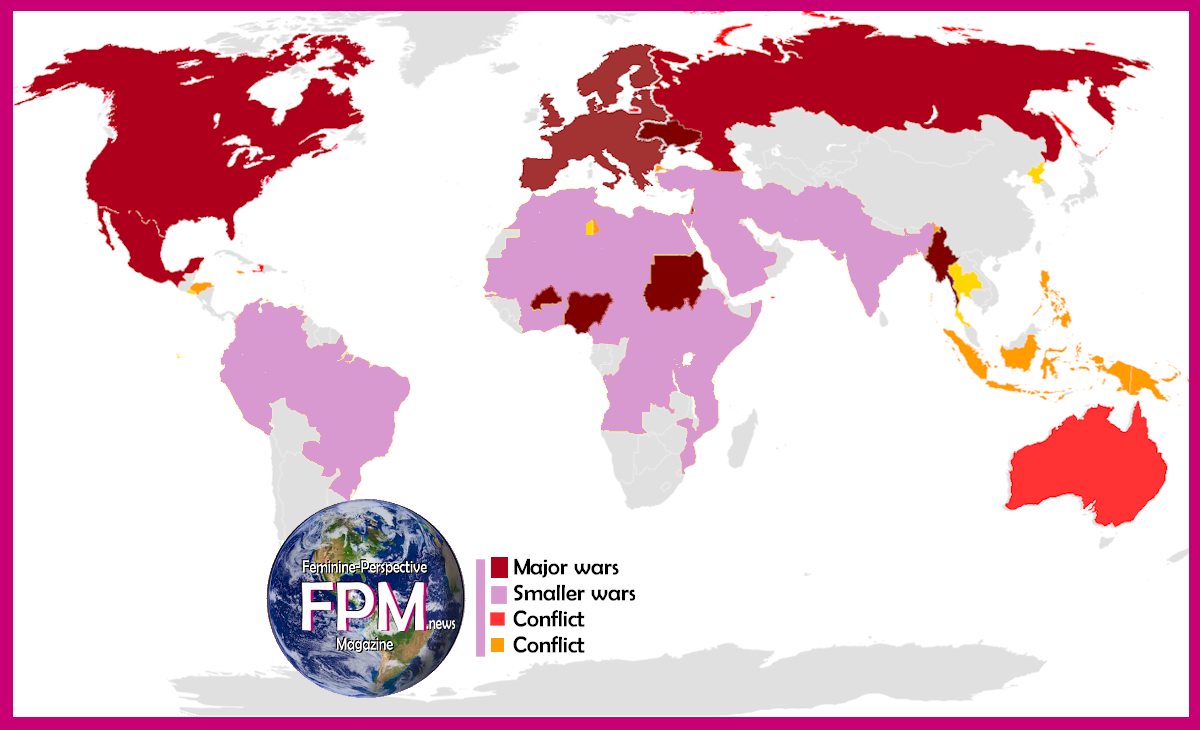
Live Updates on COVID-19 Statistics
Sources for this statistical data.
The following sources are available to readers. FPMag and The Nurses Without Borders make direct contact and interview colleagues and sources close to the information around the world to track events and statistics.